Introduction
Thalassemias are common inherited hematologic disorders worldwide, and with increasing migration, its prevalence evolves in different countries. However, community prevalence across most of the United States is unknown. Minnesota, particularly Minneapolis/St. Paul, has a relatively large community of immigrant families, with focal ethnic clusters of Karen and Hmong individuals from Southeast Asia, Liberia, and neighboring countries in Western Sub-Saharan Africa. Statewide data show that these ethnic minority populations have grown in the past decade; it is unknown whether thalassemia prevalence mirrors these migration trends. This report aims to quantify the demography and disease characteristics of children with thalassemia mutations seen at University of Minnesota/M Health Fairview (MHF) diagnosed between January 1, 2010 and December 31, 2019.
Methods
An institutional review board-approved electronic medical record (EMR) review was undertaken. Patients born on or after January 1, 2001 were included if they received medical care within the MHF system and thalassemia status could be confirmed. The prevalence by thalassemia type, demography, language, treatment details, and specialist involvement were detailed. A patient's ethnicity determination was defaulted to "American" if the ethnicity and/or immigration country of origin going back at least two generations could not be confirmed via EMR. The trends of new diagnoses over the decade were reviewed and compared to available state demography data trends. Descriptive statistical analyses were performed for the full group and by thalassemia type.
Results
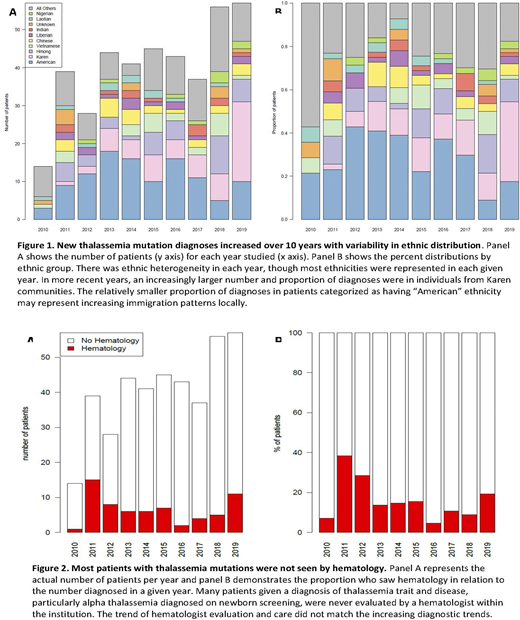
A total of 404 patients met inclusion criteria, representing 48 country or region-specific ethnicities, 17 known countries of birth, and 30 separate languages. The most prevalent immigrant ethnicities were Karen (15%), Hmong (10%), and Vietnamese (5%), representing the 14th, 2nd, and 6th-largest immigrant communities in the state, respectively (www.mncompass.org). In Minnesota, the Asian population grew by 32% (69,800 people) between 2010-2018 (Minnesota State Demographic Center, https://mn.gov/admin/demography/data-by-topic/age-race-ethnicity/). The overall number of thalassemia diagnoses also increased over the decade, with Karen patients representing the largest proportional increase over the available time frame (Figure 1).
Including both trait and disease, alpha thalassemias were more frequently diagnosed than beta thalassemias (63% versus 37%). Of the alpha thalassemias, 79% were suspected or confirmed 1-2 gene deletions based on newborn screening. Eleven (2.7%) had hemoglobin (Hb) H disease and 2 (0.5%) had alpha thalassemia major. Beta thalassemia intermedia, beta thalassemia major, and HbE were collectively 5.4% of all patients, 59% of whom were transfusion-dependent. Genetic confirmation was performed for 10.4% of all thalassemias. Those with alpha thalassemias were more ethnically diverse. Aside from those categorized as "American", those with beta thalassemias were more likely to be Karen (25%), while those with alpha thalassemias were most likely to be Hmong (14.4%). Seven had chelation prescribed during the time frame and 5 underwent bone marrow transplant. Only 16% were seen by a hematologist in the MHF system, though the yearly trends of hematology care did not match the increased diagnostic rate (Figure 2).
Conclusions
The incidence of pediatric thalassemia diagnoses have increased over the past decade at MHF, somewhat reflecting the statewide demographic trends. However, most patients are never being seen by hematology. A caveat to the data described is the fact that MHF is 1 of 2 pediatric hospitals locally, with the other having the historically larger thalassemia patient population. Thus, while these data offer crucial insights into the potential frequency of thalassemia mutations in our state, they also are likely to significantly under-represent the local prevalence. Also, the data do not reflect the prevalence in youths diagnosed prior to 2010 or the adult prevalence, for which institutional investigations are currently ongoing. These data illuminate the need to ensure adequate educational resources and financial support for these primarily non-English-speaking communities to improve awareness for families and medical providers and offset substantial medical costs for life-saving therapies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.